What Is a Diabetic Foot Ulcer?
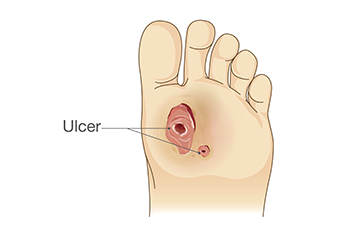
A diabetic foot ulcer is a significant and potentially serious complication arising from diabetes, characterized by open sores or wounds on the feet. The condition evolves due to a combination of factors associated with diabetes, such as impaired blood circulation, nerve damage, and compromised immune function. Elevated blood sugar levels contribute to reduced blood flow and sensation in the extremities, making the feet susceptible to injury. Minor cuts, blisters, or friction can escalate into non-healing ulcers due to the body's compromised ability to repair itself. What sets diabetic foot ulcers apart is their propensity for infection and slow healing, posing a heightened risk of severe complications if left untreated. Understanding the definition of diabetic foot ulcers underscores the importance of vigilant foot care, regular examinations, and proactive management strategies. If you have diabetes and have developed a diabetic foot ulcer, it is strongly suggested that you speak to a podiatrist who can guide you toward the best management and treatment strategies for this type of wound.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Stephen Petrofsky from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Port Charlotte, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
When Flat Feet Need a Surgical Solution
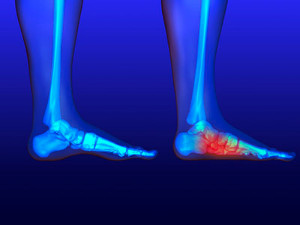
Flat feet, a condition where the arches of the feet are significantly reduced or absent, can cause discomfort and limit mobility for some individuals. While many cases of flat feet can be managed with conservative treatments like orthotics, exercises, and supportive footwear, there are situations where surgery becomes a viable option. Surgical intervention for flat feet typically aims to reconstruct and restore the arches of the feet, improving overall foot function and alleviating pain. This procedure is known as flatfoot reconstruction surgery. Podiatric surgeons may employ various techniques, such as tendon transfers, bone realignment, or the use of implants to achieve the desired results. Candidates for flatfoot surgery often include people who experience severe pain, difficulty in walking, or whose flat feet result from structural abnormalities. If you suspect you may need flatfoot surgery, it is suggested that you schedule an appointment with a podiatrist to discuss whether this is a correct option for you.
Flatfoot is a condition many people suffer from. If you have flat feet, contact Dr. Stephen Petrofsky from Florida. Our doctor will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our office located in Port Charlotte, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
Common Causes of Lateral Foot Pain

Lateral foot pain can be the result of various conditions, each with distinct features and treatments. Ankle sprains, often caused by rolling the ankle, result in ligament tears, possibly leading to side foot pain, swelling, and instability. Cuboid syndrome may be noticed after an ankle sprain as the cuboid bone shifts out of position. This can cause ongoing foot pain, especially after activity. Peroneal tendonitis, due to repetitive stress, leads to lateral foot pain that worsens with activity. Stress fractures, often caused by repeated stress from sports or increased activity, result in progressive pain during physical activity, localized swelling, and tenderness. Diagnosis relies on bone scans or MRIs, and surgery may be needed in severe cases. Bunions, caused by genetics, wearing tight shoes, flat feet, or arthritis, may lead to symptoms like a rotated big toe, pain, and deformity. Corns and calluses, characterized by thick, raised skin areas, often occur due to excessive friction from tight shoes, foot deformities, or aging. Posterior tibial tendonitis is associated with flat feet, and results from irritation and inflammation of the posterior tibial tendon. This causes pain on the inner side of the ankle and foot during activity. For help with any of the above conditions, it is suggested that you make an appointment with a podiatrist.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Dr. Stephen Petrofsky from Florida. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Port Charlotte, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
The Significance of Purple, Black, and Blue Feet in the Elderly

In the elderly, purple, black, or blue discoloration of the feet can signify underlying health issues that warrant attention. These hues may indicate poor blood circulation, potentially linked to conditions such as peripheral artery disease. Reduced blood flow can lead to tissue damage, causing the skin to take on these distinctive colors. Moreover, elderly individuals are prone to bruising, and black or blue discoloration might result from minor injuries due to thinning skin and weakened blood vessels. Another potential cause is venous insufficiency, where compromised vein function hinders proper blood return to the heart. This can result in pooling of blood in the lower extremities, manifesting as discoloration. In some cases, these symptoms may point to more serious conditions like deep vein thrombosis. It is vital for caregivers and healthcare providers to monitor such changes, promptly addressing any concerns to ensure the elderly receive appropriate medical attention and intervention for their overall well-being. If you notice these colors on the feet of elderly people you are caring for, it is strongly suggested that you consult a podiatrist who can accurately diagnose and offer effective treatment options.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact Dr. Stephen Petrofsky from Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our office located in Port Charlotte, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Elderly Foot Care
As you grow older, you will start to notice more problems with your feet due to wear and tear. This may also happen because the skin will start to become thin and lose elasticity. Some signs of aging feet are regular aches and pains, bunion development, and clawed toes.
Fortunately, there are ways you can improve comfort, relieve pain, and maintain mobility in your feet. One of the best ways to deal with aging feet is to exercise. If you keep active, your muscles will become toned which will then strengthen the arches in the foot and stimulate blood circulation.
It is important that you practice proper foot care to protect your aging feet. You should wash your feet in warm water on an everyday basis. Afterward, the feet need to be dried well and it is important to dry between the toes. Your toenails should be trimmed and kept under control; nails that are poorly cut may become ingrown. At the end of each day, performing an inspection of your feet will allow you to detect any ailments in their early stages.
As you grow older, it becomes more important that you wear comfortable shoes. Your shoes should be secure, and they should provide decent arch support. If you are looking to buy a new pair of shoes, it is best to look for a pair that are made from a breathable material. It is also helpful to have shoes that have a bit of extra room at the top of the shoe, especially if you suffer from swollen feet.
The most common foot problems that elderly people will encounter are bunions, calluses, corns, hammertoes, heel pain, and foot problems related to diabetes. Some other issues include arch pain, tarsal tunnel syndrome, Achilles tendonitis, and Morton’s neuroma
An annual foot examination is a great way for you to ensure that you do not have any serious health problems with your feet. You should talk to a podiatrist about the available treatment options for whichever foot issue you are dealing with.
Are You Suffering From Ingrown Toenails?
Congenital Foot Deformities and a Focus on Clubfoot

Congenital foot deformities, occurring at birth, present a spectrum of conditions that impact the structure and function of the feet. One notable congenital deformity is clubfoot, a condition where the foot is twisted inward and downward. This malformation results from a combination of genetic and environmental factors influencing the development of tendons, muscles, and bones in the foot during pregnancy. In clubfoot, the Achilles tendon is often shorter than usual, exacerbating the inward rotation of the foot. While the exact cause remains elusive, early identification and intervention are pivotal. Advances in medical understanding and technology continue to enhance treatment outcomes, providing hope for those born with congenital foot deformities. Those born with clubfoot can lead active and fulfilling lives with proper care and intervention. If your child has been born with clubfoot, it is strongly suggested that you consult a podiatrist who can immediately begin appropriate treatment.
Congenital foot problems require immediate attention to avoid future complications. If you have any concerns, contact Dr. Stephen Petrofsky of Florida. Our doctor can provide the care you need to keep you pain-free and on your feet.
Congenital foot problems are deformities affecting the feet, toes, and/or ankles that children are born with. Some of these conditions have a genetic cause while others just happen. Some specific foot ailments that children may be born with include clubfeet, polydactyly/macrodactyly, and cleft foot. There are several other foot anomalies that can occur congenitally. What all of these conditions have in common is that a child may experience difficulty walking or performing everyday activities, as well as trouble finding footwear that fits their foot deformity. Some of these conditions are more serious than others. Consulting with a podiatrist as early as possible will help in properly diagnosing a child’s foot condition while getting the necessary treatment underway.
What are Causes of Congenital Foot Problem?
A congenital foot problem is one that happens to a child at birth. These conditions can be caused by a genetic predisposition, developmental or positional abnormalities during gestation, or with no known cause.
What are Symptoms of Congenital Foot Problems?
Symptoms vary by the congenital condition. Symptoms may consist of the following:
- Clubfoot, where tendons are shortened, bones are shaped differently, and the Achilles tendon is tight, causing the foot to point in and down. It is also possible for the soles of the feet to face each other.
- Polydactyly, which usually consists of a nubbin or small lump of tissue without a bone, a toe that is partially formed but has no joints, or an extra toe.
- Vertical talus, where the talus bone forms in the wrong position causing other bones in the foot to line up improperly, the front of the foot to point up, and the bottom of the foot to stiffen, with no arch, and to curve out.
- Tarsal coalition, when there is an abnormal connection of two or more bones in the foot leading to severe, rigid flatfoot.
- Cleft foot, where there are missing toes, a V-shaped cleft, and other anatomical differences.
- Macrodactyly, when the toes are abnormally large due to overgrowth of the underlying bone or soft tissue.
Treatment and Prevention
While there is nothing one can do to prevent congenital foot problems, raising awareness and receiving neonatal screenings are important. Early detection by taking your child to a podiatrist leads to the best outcome possible.
If you have any questions please feel free to contact our office located in Port Charlotte, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.